Colorectal Cancer Screening
Colorectal cancer starts in cells in the colon or rectum. It's one of the main causes of cancer deaths in the U.S. But when it's found and treated early, the chances of a full recovery are very good. It needs to be found when it's still small and hasn't spread. This cancer rarely causes symptoms in its early stages. Because of this, screening for it is important. This means looking for abnormal growths before you have symptoms. Screening is even more important if you have risk factors for this cancer.
Risk factors for colorectal cancer
Your risk of having colorectal cancer is higher if you:
-
Are older. Older adults are most likely to get colorectal cancer. But it can occur at any age.
-
Have a family history or personal history of colorectal cancer or polyps
-
Are African American
-
Are of Eastern European Jewish descent (Ashkenazi)
-
Have Crohn’s disease or ulcerative colitis
-
Have type 2 diabetes
-
Have an inherited genetic syndrome, such as Lynch syndrome or familial adenomatous polyposis
-
Are overweight
-
Are not physically active
-
Smoke
-
Drink a lot of alcohol (more than 2 drinks per day for men and 1 drink per day for women)
-
Eat a lot of red or processed meat
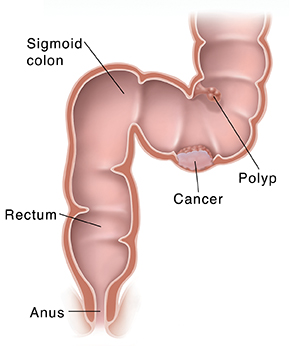
The colon and rectum
The colon and rectum are part of your digestive system. Food goes from your stomach to your small intestine. It then goes into your colon. As it travels through the colon, water is removed. The waste that is left (stool) becomes more solid. The muscles of your intestines push the stool toward the sigmoid colon. This is the last part of the colon. The stool then moves into the rectum. It's stored there until it’s ready to leave your body when you poop.
How colorectal cancer starts
Polyps are growths that can form on the inner lining of the colon and rectum. Most are benign. This means they aren’t cancer. But over time, some polyps can become cancer. These are called malignant. This happens when cells in these polyps start to grow out of control. In time, the cancer cells can spread to more of the colon and rectum. The cancer can spread to nearby organs or lymph nodes. It can spread to other parts of the body, like the liver or lungs. Finding and removing polyps early can help keep cancer from starting.
Colorectal cancer screening
Screening means looking for a health problem before you have symptoms. Screening for colorectal cancer starts with:
-
Your health history. Your healthcare provider will ask about your health history. They will ask you about possible cancer risk factors. Tell your healthcare provider if you have a family member who has had colorectal cancer or polyps. Tell them about any health problems you have had in the past.
-
Screening tests. The American Cancer Society and the U.S. Preventive Services Task Force advise colorectal cancer screening for people at average risk starting at age 45. Talk with your healthcare provider about your risks. Ask when you should start screening tests. It's also important to check with your health insurer about your coverage.
Types of screening tests
Below are the most common types of colorectal cancer screening tests. How often you should be screened depends on your risk and the test that you and your healthcare provider choose. If you have a family history of colon cancer or are at high risk for other reasons, you may need to have screening earlier or more often.
Stool testing
Fecal occult blood test (FOBT) or fecal immunochemical test (FIT) (every year)
These tests check for blood in stool that you can’t see. This is called hidden or occult blood. Hidden blood may be a sign of colon polyps or cancer. A small sample of stool is sent to a lab where it's tested for blood. Most often, you collect this sample at home using a kit your healthcare provider gives you. Make sure you know what to do and follow the directions carefully. For example, you might need to not eat certain foods and not take some medicines before collecting stool for this test. If you have an abnormal FOBT or FIT, you will likely need a colonoscopy.
Stool DNA test (every 1 to 3 years)
This test looks for cells in your stool that have abnormal DNA in them. These DNA changes might be signs of cancer or polyps. This test also looks for hidden blood in stool. For this test, you collect an entire bowel movement. This is done using a container that's put in the toilet. The kit has directions on how to collect, prepare, and send your stool. It goes to a lab for testing. If you have an abnormal result on stool DNA, you will likely need a colonoscopy.
Visual exams
Colonoscopy (every 10 years)
This test allows your healthcare provider to find and remove polyps in your colon or rectum. It is the only screening test that lets your healthcare provider see your entire colon and rectum. This test lets your healthcare provider remove any pieces of tissue that need to be checked for cancer.
One or 2 days before the test, you'll do a bowel prep. The bowel prep cleans out your colon. This is so the lining can be seen during the test. You'll be given directions on how to do the prep. It will include a liquid diet. You will then use a strong laxative solution or an enema.
Just before the test, you're given medicine to make you sleepy. Then the healthcare provider gently puts a long, flexible, lighted tube (colonoscope) into your rectum. The scope is guided through your entire colon. The provider looks at images of the inside of your colon on a video screen. Any polyps seen are removed. They are sent to a lab for testing. If a polyp can’t be removed, a small piece of it is taken out for testing. If the tests show it might be cancer, the polyp might be removed later during surgery.
Flexible sigmoidoscopy (every 5 years)
This test is a lot like a colonoscopy. But it is done only on the sigmoid colon and rectum. The sigmoid colon is the last 2 feet or so that connects to your rectum. The entire colon is about 5 feet long.
One or 2 days before the test, you'll do a bowel prep. The bowel prep cleans out your colon. This is so the lining can be seen during the test. You'll be given directions on how to do the prep. It will include a liquid diet. You will then use a strong laxative solution or an enema.
You are awake during the test. But you may be given medicine to help you relax. The healthcare provider guides a thin, flexible, lighted tube (sigmoidoscope) into your rectum and lower colon. The images are shown on a video screen. Polyps can be removed. They are sent to a lab for testing.
Another choice is flexible sigmoidoscopy every 10 years, with a FIT stool test every year. Talk with your healthcare provider to learn more.
Virtual colonoscopy (every 5 years)
This test is also called a CT colonography. It uses a series of X-rays. They make a 3-D image of your colon and rectum.
One or 2 days before the test, you'll do a bowel prep. The bowel prep cleans out your colon. This is so the lining can be seen during the test. You'll be given directions on how to do the prep. It will include a liquid diet. You will then use a strong laxative solution or an enema.
During the test, you'll lie on a narrow table that's part of an X-ray machine called a CT scanner. A soft, small tube will be placed into your rectum. This will fill your colon and rectum with air. The table will slide into the CT scanner. A series of X-rays will be taken. A computer will combine these to create a 3-D image. Because the test uses X-rays, it exposes you to a small amount of radiation. This test can be done without sedation. If polyps or any other changes are seen, you'll need a colonoscopy. This is done so the tissue can be removed for testing.
Talking with your healthcare provider
Talk with your healthcare provider about which screening tests might be best for you. Each test has pros and cons. But no matter which test you have, the most important thing is that you get screened. If cancer is found at an early stage during screening, it's easier to treat. And treatment is more likely to work well. Cancer can even be prevented with routine screening tests.
If you have a screening test other than a colonoscopy and have an abnormal test result, you'll need to follow-up with colonoscopy. This would not be considered a screening colonoscopy. Your deductible and co-pay may apply. Check with your health insurer so you know what to expect.
Ask your healthcare provider about your level of risk. You may need to be screened on a different schedule if you are at higher risk of this cancer. Talk with your provider about your health history to decide on the screening plan that's best for you.