Distal Ureterectomy
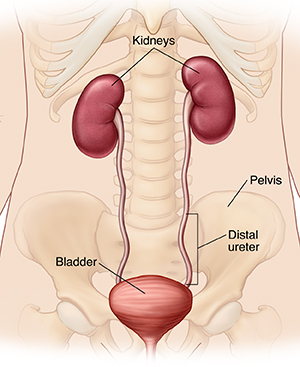
The ureters are tubes that connect and drain urine from the kidneys to the bladder. Cancer has been found in the lower (distal) part of one of your ureters. To treat the cancer, a distal ureterectomy is done. This surgery removes the lower part of the ureter and part of the bladder.
Getting ready for surgery
Prepare for the surgery as you have been told. In addition:
-
Tell your healthcare provider about all medicines you take. This includes prescription and over-the-counter medicines, vitamins, herbs, and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery, as directed by your healthcare provider.
-
Follow any directions you are given for not eating or drinking before surgery. If you have been directed to take medicines, take them with a small sip of water.
Two types of surgery
The surgery may be done through several small cuts (laparoscopy) or through one larger cut (open surgery). Laparoscopy is not always possible in all cases. In some cases, your surgeon may start surgery using laparoscopy but may change to open surgery for safety reasons. You and your surgeon will discuss your options.
-
Laparoscopy. The surgeon makes several small cuts (incisions) in the belly (abdomen). The scope is put through one of the small incisions. The scope sends pictures from inside the belly to a video screen. Surgical tools are placed through the other incisions. The surgeon may use a method called robotic laparoscopy. The robotic system gives a 3-D view inside the body. It also helps the surgeon’s hand movements.
-
Open surgery. One larger incision is made in the side. The surgeon does the surgery through this larger incision.
The day of surgery
The surgery takes about 2 to 3 hours. Afterward, you will stay in the hospital for 1 to 3 nights.
Before the surgery begins:
-
An IV (intravenous) line is put into a vein in your arm or hand. This line delivers fluids and medicines (such as antibiotics).
-
You may get medicine to prevent blood clots.
-
To keep you pain-free during the surgery, you’re given general anesthesia. This medicine allows you to sleep through the surgery. A tube may be put into your throat to help you breathe.
-
A thin tube (catheter) is placed into your bladder through the urethra. This drains urine during the surgery and for a time afterward.
During the surgery:
-
The area is checked for cancer spread. If any is seen the procedure may be stopped.
-
The lower end of the ureter and part of the bladder are removed. Nearby lymph nodes may also be removed. The remaining ureter is then reinserted into the bladder and sewn into place.
-
A long, flexible tube called a stent is put into the ureter. It reaches from the kidney into the bladder. It is kept in place for 4 to 6 weeks after surgery to help hold the ureter open while it heals.
-
The catheter may be left in the bladder to drain urine while the bladder heals.
-
When the surgery is finished, all tools are removed. The incision or incisions are closed with stitches, staples, surgical glue, or strips of surgical tape. One or more tubes (drains) may be placed into the incision site. These drain fluid that may build up as healing starts.
Recovering in the hospital
After the surgery, you will be taken to the PACU (post anesthesia care unit). There you will be closely watched as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube were used, your throat may be sore at first. When you are ready, you will be taken to your hospital room. While in the hospital:
-
You will be given medicine to manage pain. Let your providers know if your pain is not controlled.
-
The catheter in your urethra and any drains will likely be removed before you leave the hospital. If not, you will be told how to care for them at home.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days, to help care for you. Recovery time varies for each person. Your healthcare provider will tell you when you can return to your normal routine. Until then, follow the instructions you have been given. Make sure to:
-
Take all medicines as directed.
-
Care for your incisions as instructed. If you’re sent home with a catheter or drains, take care of these as you were shown.
-
Follow your provider’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that will cover the incision with water until the provider says it’s OK.
-
Don't do strenuous activity, as advised by your provider.
-
Don't drive until your provider says it’s OK. Don't drive if you’re taking medicines that make you drowsy or sleepy.
-
Don't strain during a bowel movement. If needed, take stool softeners as directed by your provider.
The stent in your ureter will cause the urge to pass urine more often. You may also have some burning and blood in your urine. This is normal and will go away once the stent is removed during a follow-up visit.
When to call your healthcare provider
Call your healthcare provider right away if any of the following occur:
-
Fever of 100.4° F ( 38°C ) or higher, or as directed by your healthcare provider
-
Bleeding or a large amount of drainage from an incision
-
Symptoms of infection at an incision site such as increased redness or swelling, warmth, worsening pain, or bad-smelling drainage
-
Large clots of blood in your urine
-
Leg pain or swelling
-
Pain that’s not controlled with medicine
-
Inability to urinate
-
Vomiting that doesn’t go away
Call 911
Call 911 if you have:
-
Chest pain
-
Trouble breathing
Follow-up care
You will have follow-up visits with your surgeon. If stitches or staples need to be removed, this is done 7 to 14 days after surgery. The stent in your ureter will be removed in 4 to 6 weeks. You will also have regular follow-up visits with your provider to be sure the cancer doesn’t return or spread. If any further cancer treatments are needed, your provider can tell you more.
Risks and possible complications
All procedures have some risk. Possible risks of this procedure include:
-
Bleeding. This may need a blood transfusion.
-
Infection
-
Urine leakage from the ureter or bladder
-
Stricture (narrowing) in the ureter
-
Damage to the bladder, bowels, or other organs
-
Blood clots
-
Kidney damage
-
Tumor seeding. This means tumor cells that may grow into new tumors.
-
Risks of anesthesia. The anesthesiologist or nurse anesthetist will discuss these with you.