Having Laparoscopic Colon Surgery
You and your healthcare provider may decide that laparoscopic colon surgery is right for you. How well you get ready for the surgery can affect its success. For instance, proper bowel prep is an essential step in preparing for this procedure. Make sure you understand all instructions your provider gives you. If you’re not sure about what to do, ask.
Getting ready a few weeks before surgery
-
Have an exam. Have a full physical exam before surgery, as instructed by your provider. This checks the health of your heart and lungs.
-
Ask about medicines. Tell your surgeon about all the medicines you take. Ask if you should stop taking any of them. This includes prescription medicines, as well as aspirin, ibuprofen, and other over-the-counter medicines. Tell your surgeon about any herbs, illegal drugs, vitamins, or supplements you take.
-
Quit smoking. If you smoke, do your best to quit now. Smoking raises your risks during surgery. It also slows healing. Do not smoke the day of the procedure.
-
Share your alcohol history. If you drink alcohol, let your provider know how much you drink. This is very important if you are a heavy drinker or have had alcohol withdrawal symptoms in the past. Alcohol withdrawal can be dangerous. But symptoms can be safely handled if your healthcare team knows about your alcohol history.
Getting ready the day before surgery
Follow any directions you are given, including those for:
The day of surgery
When you get to the hospital, you will be asked to fill out certain forms. You will then change into a gown. An IV (intravenous) line will be put into your hand or arm. This gives fluids and medicines. You’ll meet with your anesthesiologist or nurse anesthetist to talk about the medicine that helps you sleep during surgery. Ask any questions you have at this time. Before surgery starts, you’ll be given general anesthesia to put you into a deep sleep. A soft tube (catheter) may be placed into your bladder to drain urine.
If open surgery is needed
During the procedure, the surgeon may find that it is safer to change to open surgery. This method uses a single, larger cut (incision) instead. In most cases, this change happens because of something that could not be seen on scans done before the surgery. It doesn’t mean that anything went wrong. Changing to open surgery is done to give you the best result.
During your surgery
-
Your surgeon makes several small cuts.
-
A long, thin tube (laparoscope) is then placed into one of the small cuts. This lets your surgeon see your colon on a video screen.
-
The surgical tools are placed into the other cuts. (A larger cut may be made later to take out a part of the colon.)
-
The problem part of the colon is removed (resected). Sometimes the two ends of the colon are joined. This is called an anastomosis.
-
Once surgery is done, you’ll be taken to the post anesthesia recovery unit (PACU).
Possible benefits of laparoscopic surgery
Types of colon resection
The idea of having part of your colon taken out may sound scary. But part or all of the colon can be taken out without causing serious problems. After the part of the bowel is taken out, the two ends are then reconnected (anastomosis). Below are some of the surgeries that can be done on the colon. The type of surgery depends on where the problem is in your colon.
After certain types of surgery, the colon and rectum may need to be free of stool while they heal. In other cases, the rectum has been taken out or can't be reconnected to the rest of the colon. In either case, a colostomy is needed. This makes a new opening in your belly (abdomen) so waste can leave your body. You may need the new opening for a short time or permanently. Your healthcare provider will help you learn how to care for it.
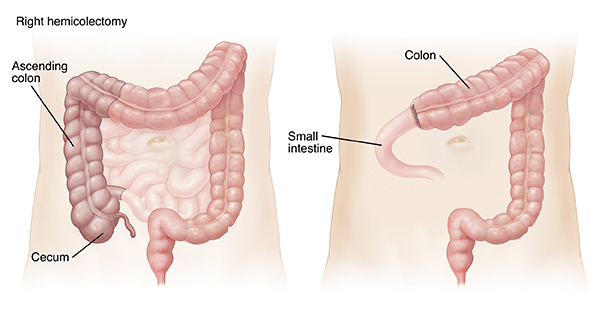 |
| Right Hemicolectomy: Part or all of the ascending (right side) colon is removed. The remaining colon is then reconnected to the small intestine. |
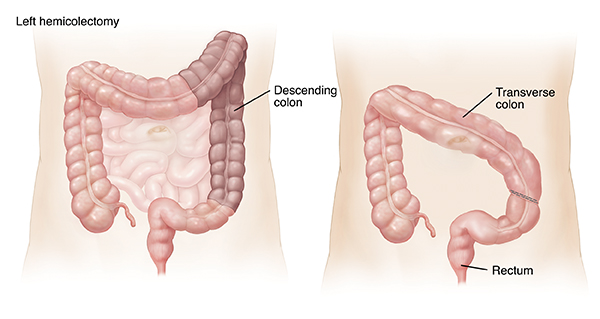 |
| Left Hemicolectomy: Part or all of the descending (left side) colon is removed. The remaining colon is then reconnected to the rectum. |
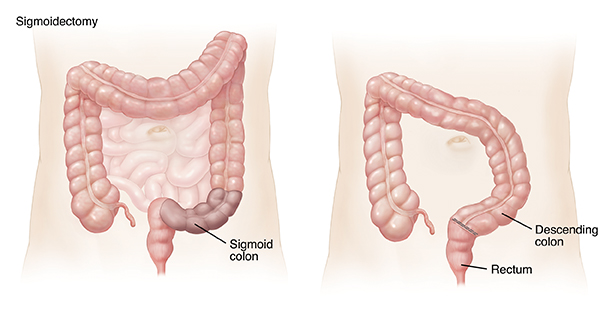 |
| Sigmoid Colectomy (Sigmoidectomy): Part or all of the sigmoid colon is removed. The descending colon is then reconnected to the rectum. |
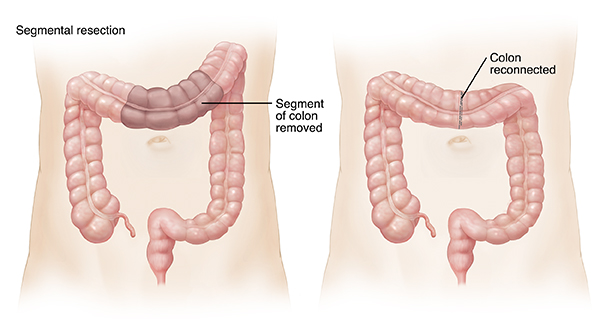 |
| Segmental Resection: One or more short segments of colon are removed. The remaining ends of the colon are reconnected. |
Risks and possible complications
Risks and possible complications of colon surgery include:
-
Infection
-
Injury to nearby organs
-
Leaking or separation after the two ends of the colon are joined (anastomosis)
-
Blood clots
-
Bleeding
-
Risks of anesthesia
-
Abscess formation
-
Bowel muscles slow or stop, and gas and waste don’t move through the body (short-term ileus)