When Your Child Needs a Tracheostomy
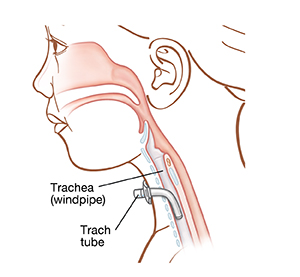
Your child's healthcare provider has told you that your child needs a tracheostomy. This creates a new pathway for air. Surgery is needed to do this. During the surgery, the surgeon makes a small opening in your child’s neck. A tube (called a trach tube) is placed in this opening. Air then flows into and out of the trach tube, allowing your child to breathe. This sheet will help you learn more about tracheostomy.
Reasons for a tracheostomy
A tracheostomy may be temporary (used for a short time) or permanent. Here are some possible reasons for a tracheostomy:
-
Need for long-term use of a ventilator (a machine that helps with breathing)
-
Obstruction in the airway due to an accident, paralysis, surgery, or malformation
-
The need for frequent suctioning of secretions in the airway
-
Obstruction of the airway during sleep (sleep apnea)
How your child’s tracheostomy works
The surgery is done in an operating room or intensive care unit (ICU). Your child will be given medicine to make them sleep during the procedure. The surgeon creates a small opening in the neck, called a stoma. The trach tube is put into the stoma. One end of the trach tube rests outside the stoma. The other end rests inside the windpipe (trachea). When your child breathes in, air goes through the tube into the trachea to the lungs. When your child breathes out, air comes out of the trach tube. Your child can still also breathe in and out through their nose.
Helping your child adjust to a tracheostomy
Depending on your child’s age, it may take some time to adjust to a tracheostomy. You can help by becoming skilled in trach tube care. Before you leave the hospital, your healthcare team can help you understand how a trach tube works and teach you how to care for it. Some things you may learn include:
-
The type, size, and length of the trach tube
-
How and when to suction
-
How to clean the area around the tube and the tube itself
-
When and how to change the trach tube
-
Signs of breathing distress and what to do
-
Signs of infection and skin breakdown and what to do
Ask your healthcare provider about home nursing care for support in the care of your child's trach tube. Make sure you've been given a home care instruction manual for tracheostomy before you leave the hospital. Also get contact information for a medical equipment supply company and a checklist of emergency supplies.
Learning as much as you may help you stay relaxed. It will help your child remain calm if there's a problem. For example, if your child feels like gagging, help them relax. Have your child breathe in slowly and deeply. Here are some other ways to help your child:
-
Eating. Follow any instructions you’re given about eating and drinking. Once your child is able to eat, encourage them to eat slowly and chew thoroughly.
-
Talking. Your child may need speech therapy to learn how to make talking easier. Some children benefit from a speaking valve, which allows speaking with greater volume. It takes some time to adjust to the valve. If your child can’t talk, help them learn new ways to communicate—with flash cards, a small whiteboard, sign language, hand gestures, or facial expressions.
-
Bathing. Make sure your child keeps the trach tube dry when bathing. You must watch your child while bathing, and don’t allow showering. To wash the hair, hold their head back, carefully supporting the head and neck. Keep water away from the trach tube.
-
Being outside. In dirty or dusty areas, cover the trach tube with an artificial nose, also called a humidity exchanger. It contains a small filter. Avoid sandboxes and beaches. Stay inside on very cold or windy days.
-
Playing. Supervise play with other children to prevent items being put into the trach tube or the trach tube getting pulled on. Don't allow contact sports or water activities.
Signs of a blocked or dislodged trach tube
These are signs that a trach tube is blocked or dislodged:
-
Trouble breathing, rapid breathing, or no breathing at all
-
Gasping, grunting, wheezing, or whistling sound when breathing
-
Restlessness
-
Flared nostrils
-
Sweaty, clammy skin
-
Anxious or frightened look
-
Pale or blue color around lips, mouth, or fingernails
-
Skin between the ribs, in the hollow of the front of the neck, or under the breastbone pulls in with each breath
If the trach tube is blocked
Ask your child's healthcare provider whether you need to keep a resuscitation bag nearby and when and how to use it. Keep a smaller-sized trach tube on hand as a backup. If there are signs of a blockage, first suction out the trach tube. If the tube is still blocked, change the trach tube and suction again. If your child continues to have trouble breathing or loses consciousness, call 911 or emergency services right away.
When to call your child's healthcare provider
Make sure you have contact information from your healthcare provider and know what numbers to call, even on evenings and weekends.
______________________________________
______________________________________
______________________________________
Call your child's healthcare provider right away if your child has any of the following:
-
Red or painful stoma
-
Small amount of bleeding from or around the tube that stops promptly
-
Yellow or green, smelly, bloody, or thick mucus from the stoma
-
Fever of 100.4° F ( 38°C) or higher, or as directed by your child's healthcare provider
-
Pain when you suction the trach tube
-
Vomiting
-
Trach tube or suction catheter that is difficult to insert
Call 911
-
Call 911 if any of the following occur:
-
Shortness of breath or any trouble breathing
-
Swelling around the trach tube
-
Large amount of bleeding, or persistent bleeding, from the trach tube